It happened with all the subtlety of a balloon deflating at a child’s birthday party: on October 6, 2025, the Centers for Disease Control and Prevention decided that the era of sweeping, one-size-fits-all COVID vaccine guidance is officially over. No more “everyone six months and up gets a shot” slogans. No more universal calendar reminders. Instead, the agency has replaced the billboard with a post-it note scrawled “ask your doctor, maybe.” It’s called “shared clinical decision-making,” which is government code for “we’d rather not be yelled at anymore, so you two figure it out.”
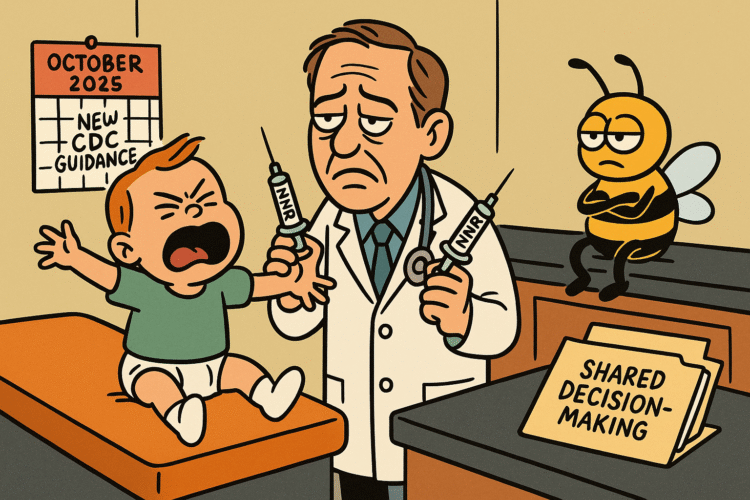
At the same time, in a quieter—but to parents far more immediate—pivot, the CDC told pediatricians to stop handing toddlers a combined MMRV shot (measles, mumps, rubella, and varicella in one syringe) at the 12–15 month visit. Too many fevers that lead to seizures, they admitted, and while the risk is still rare, they’ve decided to split the shot into two: MMR in one arm, chickenpox in the other. Parents can still choose the combo later, at the 4–6 year booster, when kids are sturdier and the odds of a seizure are lower. Toddlers, in other words, will now face double the crying and double the lollipops.
The Timeline Nobody Asked For but Everyone Gets
Here’s how it went down. In mid-September, the CDC’s vaccine advisors (the Advisory Committee on Immunization Practices, or ACIP, which sounds more like a name for a hedge fund than a public health panel) voted on two fronts: (1) loosen the COVID guidance, (2) separate the toddler shots. On October 6, the CDC stamped both votes into law, updating the official national immunization schedule. Insurers, schools, clinics, pharmacies—everyone now has to scramble to update paperwork, registries, and electronic health records that were already taped together like a college student’s first apartment.
The New Language: A Case Study in Bureaucratic Poetry
Once upon a time, the CDC issued blanket recommendations. “Everyone six months and older should get a COVID vaccine.” Short, clear, hard to argue with (well, unless you were Facebook). Now the agency has embraced a philosophy ripped from a graduate seminar: individualized, risk-based, patient-centered “shared clinical decision-making.” Which means every COVID shot will now be negotiated like a prenup. Are you at risk? Do you live with someone who’s high risk? Did you already get COVID three times and build your immunity in the dark alley of survival of the fittest? Sit down, make an appointment, and let your doctor mediate.
That is, if you can get an appointment. Because shared decision-making isn’t just a slogan, it’s a time sink. Appointments that once included a quick jab now require extended counseling, documentation, and explanations. Which means longer wait times, crankier patients, and more insurance claims that look like novels.
The Pediatric Shake-Up: One Shot Becomes Two
The second change, the MMRV split, is less existential but more immediately visceral. For decades, parents at the 12-month well-child visit endured the dreaded double injection day, but the MMRV combo spared them an extra poke. Now, that reprieve is gone. The data show toddlers between 12 and 15 months have a slightly higher risk of febrile seizures if they get the four-in-one shot. So the CDC has chosen to err on the side of safety, even if it means more tears, more Band-Aids, and more parents practicing their “you’re so brave” voice.
The combo is still available for the 4–6 year booster, because by then kids can handle the fever risk better, and also because five-year-olds can be bribed with Happy Meals. But the toddler set will be split, like a band on a farewell tour.
Operational Ripples: Everyone Gets Homework
The ripple effects started immediately. Insurers now need to update forms and clarify coverage: does “case-by-case” mean you’ll pay for the extra counseling time or leave patients holding the bill? State vaccine registries need to revise drop-down menus. Pediatric practices have to train staff, rewrite protocols, and tweak electronic health record systems so the “give MMRV” button doesn’t accidentally override the new guidance. Pharmacies, who had gotten used to blanket orders for COVID vaccines, now face the prospect of playing amateur therapist, explaining nuanced risk profiles at the drive-thru window.
The Vaccines for Children program will continue to provide free doses, but families must now wade through individualized consultations to access them. This is meant to “empower” parents, though in practice it means extra paperwork, longer visits, and a crash course in epidemiology while trying to keep a squirming toddler from licking the exam table.
The Schoolyard Question
And what about schools and daycares, those gatekeepers of herd immunity? That’s the part nobody has answered yet. States decide whether to adjust school-entry vaccine requirements. Will loosening federal COVID guidance lead some states to drop mandates altogether? Or will they keep rules intact and risk an even bigger political fight with parents who wave the new CDC language like a hall pass? For measles, mumps, and varicella, school rules are unlikely to change—the split dose is still the same coverage, just given with more Band-Aids. But the COVID side is murkier, and every politician looking for a campaign wedge issue just got a gift basket.
The Doctors’ Rebuttal Choir
Medical societies rushed to reassure the public. Yes, they said, COVID still poses serious risks, especially to older adults, immunocompromised people, and those with chronic illnesses. Yes, vaccines still prevent severe disease and death. The shared decision-making model, they stressed, isn’t a retreat—it’s a shift in communication strategy. Doctors will still strongly recommend the vaccine for high-risk groups, they just won’t say “everyone, period.” Which is like a parent saying “I strongly suggest you clean your room, but it’s your decision.” We all know how that story ends.
The Opponents’ Victory Lap
Predictably, vaccine skeptics pounced. For years they’ve argued the CDC’s universal guidance was overreach, unsupported by individual risk profiles. Now they have a soundbite: the agency agrees. The move will be touted as proof that mandates were always excessive, that the science was never settled, that Big Government finally admitted defeat. It doesn’t matter that the decision was rooted in nuance, not reversal. In the echo chamber, nuance gets flattened into meme.
The Supporters’ Counterpoint
Supporters, meanwhile, argue the change could improve trust by meeting people where they are. Shared decision-making might slow the conveyor belt but restore confidence. If parents feel their concerns are heard, they may be more likely to say yes. That’s the hope, anyway. The risk is that instead of tailoring trust, the policy depresses uptake in a year already marked by measles outbreaks and a public still polarized over who needs which shots and when.
The Practical “What Now”
For the average parent or patient, here’s what it means:
- Expect longer conversations at your doctor’s office if you want a COVID booster. It won’t be “you’re due, roll up your sleeve.” It will be “let’s talk about your risk factors.”
- Insurance claims will get more complicated. If your appointment takes twenty minutes longer, will your copay take a hit too? The fine print is still being written.
- At the 12- and 15-month well-child visits, your toddler will now get two shots instead of one. Parents should prepare to comfort, distract, and bribe accordingly.
- At ages 4–6, the combo shot is still an option, so at least kindergarteners can consolidate their trauma.
- Clinics and health systems will retrain staff, update electronic records, and track data on uptake and febrile seizures. Expect a flurry of “workflow updates” from pediatric offices in the coming weeks.
And for everyone else: brace for another round of debates, memes, and late-night monologues about how the CDC can’t make up its mind.
The Stakes
This is not just paperwork. The real stakes are whether the new model increases trust or feeds apathy. Will parents who were already hesitant lean further away now that the government isn’t telling them “everyone, period”? Will shared decision-making improve tailored care, or will it fracture the fragile herd immunity we’ve been taping together since 2020? Will measles outbreaks in under-vaccinated communities continue to flare, and will COVID become another seasonal nuisance we half-ignore, like potholes or the state of Congress?
The data will tell the story over the coming months. Uptake rates, outbreak reports, febrile seizure incidence—all will be watched like a reality show nobody wanted but everybody has to live in.
When Guidance Turns Into Guesswork
The CDC insists this is progress, a more nuanced, patient-centered approach. But nuance is exhausting in a culture that treats nuance like a mosquito buzzing in the bedroom at night. Parents want clarity, not philosophy. Clinicians want efficiency, not extended counseling sessions that double their documentation load. And the public, already bone-tired of pandemic whiplash, hears “shared decision-making” as “you’re on your own, good luck.”
Maybe this shift will rebuild trust. Maybe it will deepen skepticism. Either way, the agency has rolled out a new era of individualized immunization that looks less like a public health playbook and more like speed dating: you sit down, you explain your history, your risk, your preferences, and you hope it ends without regret.
Public health was once about clear, collective rules. Now it’s about negotiated settlements. And in that gap—between the universal and the individualized—sits a virus that doesn’t care how nuanced the conversation is.